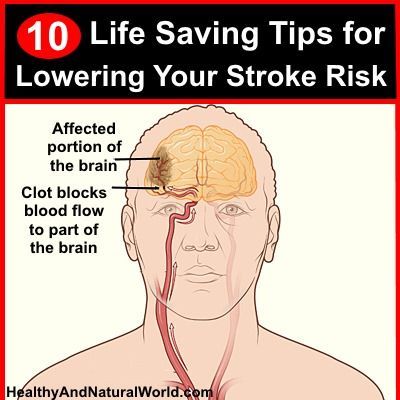
Stroke is a serious medical condition that occurs when the blood supply to the brain is disrupted or reduced, resulting […]
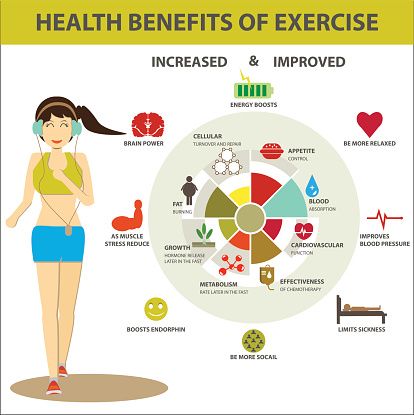
Benefits of Regular Exercise for Well-being
Regular exercise offers a wide range of benefits for overall well-being. One of the most significant advantages is improved physical […]
Diabetes Prevention: Lifestyle Changes that Matter
Diabetes has become a global epidemic, affecting millions of people worldwide. This chronic condition not only impacts an individual’s health […]
Importance of Regular Gynecological Check-ups
Gynecological check-ups are an essential part of every woman’s healthcare routine. These regular visits to a gynecologist help ensure optimal […]
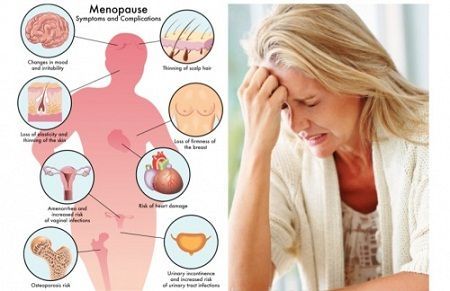
Common Women’s Health Concerns and Solutions
Women’s health is a vital aspect of overall well-being. However, various concerns can arise that require attention and appropriate solutions. […]
Understanding Common Health Issues
Good health is essential for overall well-being and a happy life. However, many individuals experience common health issues that can […]
Navigating Menopause with Confidence
Menopause is a natural stage in a woman’s life that marks the end of her reproductive years. While it is […]
Breast Health: Screening and Self-Exams
The importance of breast health cannot be emphasized enough. Regular screening and self-exams play a significant role in early detection […]
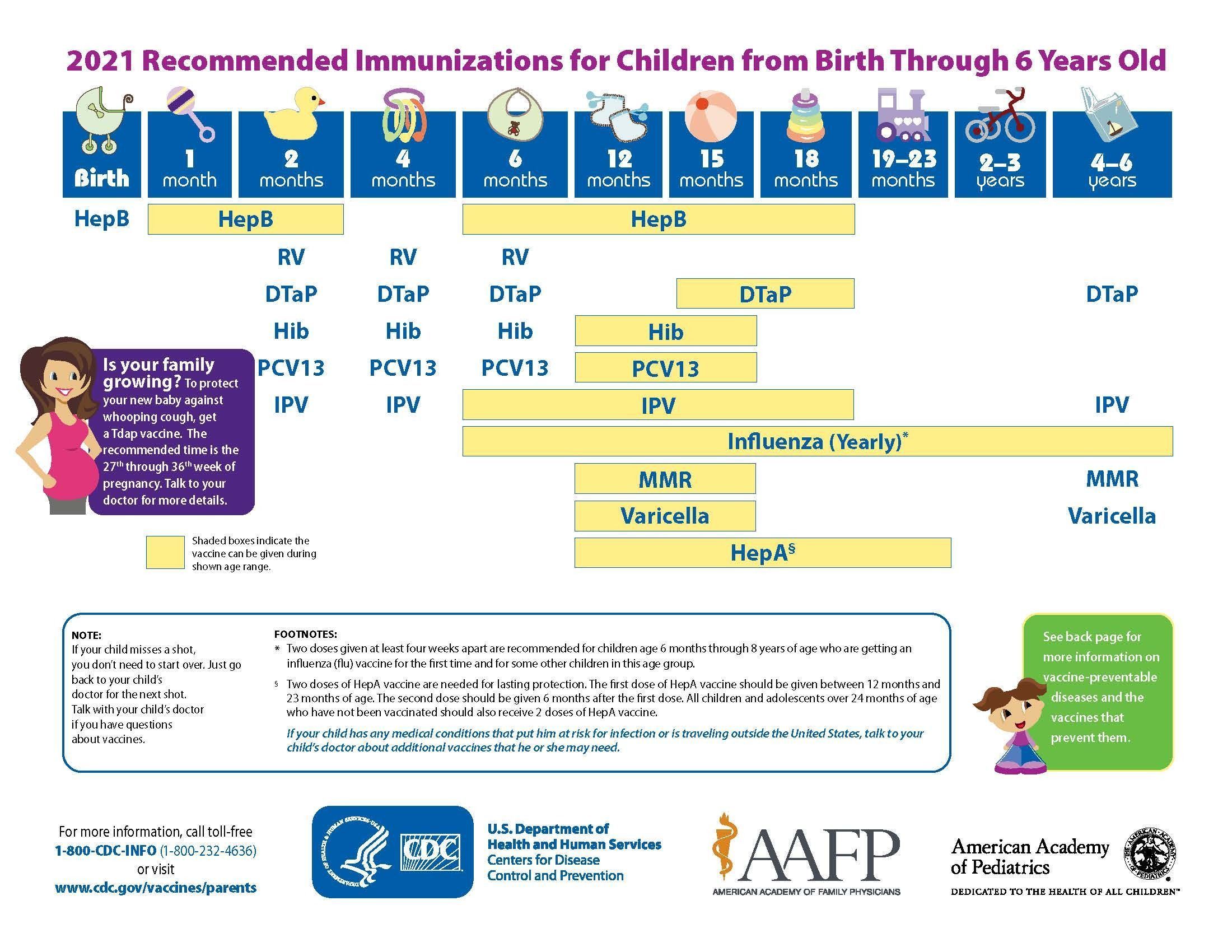
Vaccination Importance and Schedule
Vaccination plays a crucial role in safeguarding public health by preventing the spread of infectious diseases. Vaccines have been instrumental […]
Postpartum Care: Taking Care of Mom and Baby
During the postpartum period, it is essential to focus on the well-being of both the mother and the newborn baby.